A Growing Epidemic: Diabetic Retinopathy and the Global Threat to Vision
Diabetic retinopathy (DR) is a serious eye disease and a leading cause of blindness that results when diabetes' sustained high blood sugar levels cause damage to the retina – the part of the eye that detects light – over time. This damage can manifest in a multitude of ways, ranging from inflammation to the overgrowth of abnormal blood vessels. Affecting approximately 103 million diabetic patients worldwide in 2020, this number is projected to rise to 129.84 million by 2030 and a staggering 160.50 million by 2045.
The Western Pacific, Middle East and North Africa, and North America and Caribbean are expected to be the regions most impacted by this growing health crisis.
Unraveling the Complexities of Diabetic Retinopathy
DR develops over time as diabetes progresses. The chronic high blood sugar levels lead to a cascade of damaging processes within the retina, affecting its delicate blood vessels and eventually leading to vision loss. This intricate process is driven by several key mechanisms, including:
Polyol Pathway
Elevated blood glucose levels activate the polyol pathway, where glucose is converted to sorbitol. Sorbitol, being hydrophilic, causes intracellular osmotic imbalance, damaging retinal cells. This process also leads to the production of fructose, which further contributes to oxidative stress and cellular damage via the formation of Advanced Glycation End Products (AGEs).
Accumulation of AGEs
AGEs contribute to the damage by promoting oxidative stress, which in turn impairs the function of vital proteins and leads to inflammation. The accumulation of AGEs also reduces the production of Pigment Epithelium-Derived Factor (PEDF), a protective molecule, further exacerbating the damage.
Protein Kinase C (PKC) Activation
Elevated blood glucose also activates Protein Kinase C (PKC), specifically the PKC-δ isoform. This activation leads to a decline in the signaling of Platelet-Derived Growth Factor (PDGF) receptors, which are crucial for the survival of pericytes, cells that support the blood vessels. The loss of pericytes weakens the blood vessels, making them more susceptible to leakage and ultimately contributing to the development of DR.
Oxidative Stress
High blood glucose levels also create oxidative stress in the retina. This is caused by the production of reactive oxygen species (ROS), which damage DNA and cellular components. This oxidative stress further amplifies the inflammatory cascade, contributing to the breakdown of the blood-retinal barrier (BRB) and leading to retinal inflammation.
The Role of Pericytes and Endothelial Cells
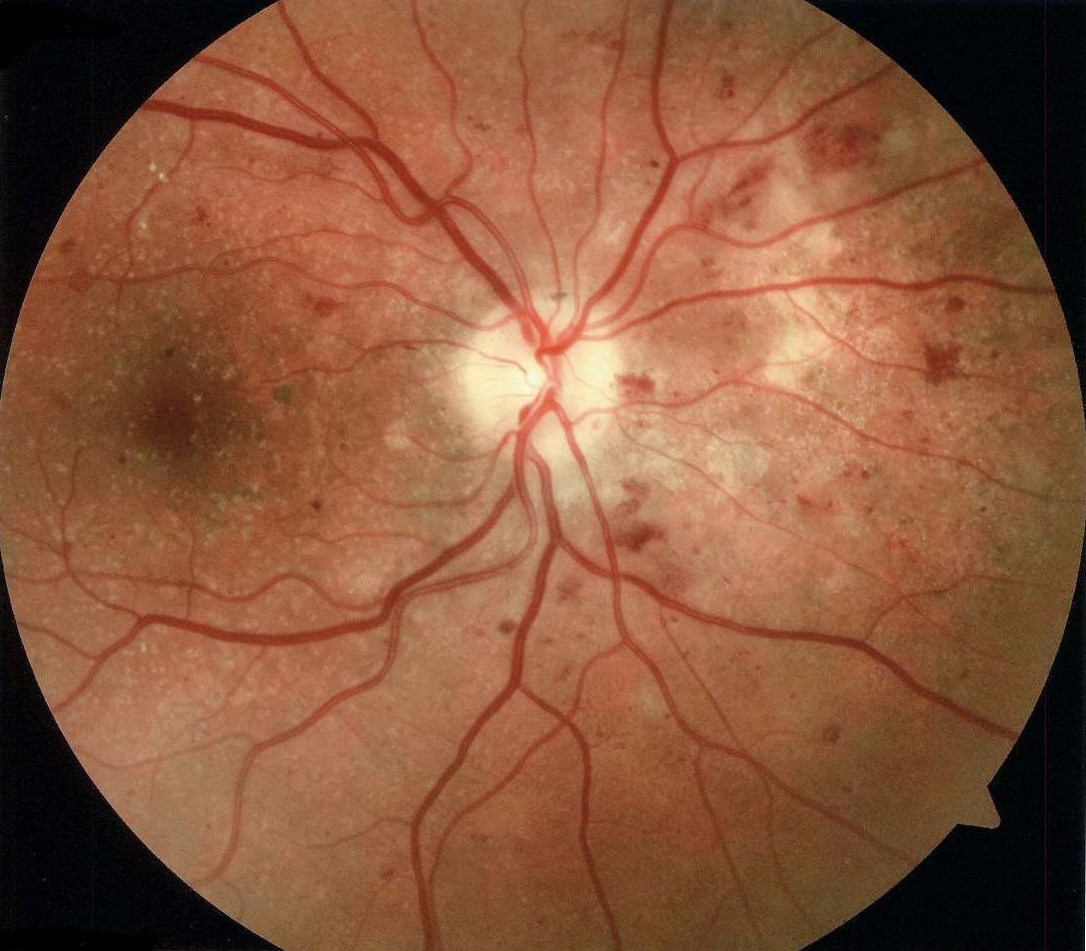
The loss of pericytes is a hallmark of early-stage DR. These cells play a crucial role in maintaining the integrity of the blood vessels. The damage to pericytes, combined with the breakdown of the BRB, leads to capillary occlusion, resulting in retinal ischemia. This ischemia further exacerbates the damage, leading to the formation of microaneurysms, hemorrhages, and cotton wool spots.
Retinal Neovascularization: A Desperate Attempt at Repair
In an attempt to compensate for the loss of blood supply, the retina undergoes neovascularization, forming new and abnormal blood vessels. This process is triggered by hypoxia (oxygen deficiency) and is mediated by the upregulation of Vascular Endothelial Growth Factor (VEGF). However, these new vessels are fragile and prone to leakage, contributing to further damage and potentially leading to retinal detachment.
Neurodegeneration: The Final Stage
As the disease progresses, neurodegeneration sets in. The loss of neurotrophic factors like NGF (nerve growth factor), PEDF, and IRBP (interphotoreceptor retinoid-binding protein) disrupts the delicate balance of the retina, leading to neuronal death.
The Importance of Early Detection and Prevention
DR is typically asymptomatic in its early stages. Regular eye examinations, particularly for individuals with diabetes, are crucial for early detection. Early intervention is key to reducing the risk of vision loss. Controlling blood glucose levels, maintaining a healthy blood pressure, and managing lipids are vital for slowing down the progression of DR.
Treatment Options for Diabetic Retinopathy
Treatment for DR depends on the severity of the condition. The most common treatment modalities include:
Laser Photocoagulation
Laser photocoagulation is used to destroy the abnormal blood vessels that contribute to leakage and fluid buildup. This treatment is effective in reducing the risk of vision loss in patients with high-risk PDR and severe NPDR.
Anti-VEGF Injections
Anti-VEGF injections are used to inhibit the growth of abnormal blood vessels and reduce leakage. These injections are particularly effective in treating DMO (diabetic macular edema), which is a common complication of DR.
Intravitreal Corticosteroids
Intravitreal corticosteroids can be used to reduce inflammation and fluid buildup in the retina. They are particularly helpful in patients who have not responded well to laser photocoagulation or anti-VEGF injections.
Vitrectomy
Vitrectomy is a surgical procedure used to remove the vitreous gel from the eye. This procedure is often performed in cases of PDR where severe fibrovascular proliferations have led to retinal detachment.
The Future of Diabetic Retinopathy Treatment: Targeting IL-6
Researchers are exploring novel treatment approaches, focusing on the inflammatory processes that drive DR. One promising target is Interleukin-6 (IL-6), a cytokine that plays a key role in inflammation. By selectively blocking the trans-signaling pathway of IL-6, researchers hope to reduce inflammation and prevent further damage to the retina.
Understanding IL-6 Signaling
IL-6 is a complex protein with both beneficial and harmful effects. Its trans-signaling pathway is primarily responsible for the harmful inflammatory effects, while cis-signaling is involved in regenerative processes.
Targeting IL-6 Trans-Signaling
By using drugs like sgp130Fc, which specifically block IL-6 trans-signaling, researchers aim to dampen the inflammatory response while preserving the beneficial effects of cis-signaling. Early studies suggest that this approach can effectively balance the levels of VEGFA and VEGFB in the retina, potentially mitigating the damage caused by DR.
Embracing a Proactive Approach to Protect Your Vision
DR is a serious but preventable condition. Regular eye exams, strict blood sugar control, and a healthy lifestyle are essential for protecting your vision and reducing your risk of developing DR. If you have diabetes, be sure to discuss your risk factors with your doctor and take proactive steps to manage your health.
Beyond the Eye: Systemic Implications of Diabetic Retinopathy
DR is not just an eye disease; it is a systemic condition that reflects the damaging effects of diabetes throughout the body. Individuals with DR are at increased risk of developing other diabetes-related complications, including:
Neuropathies
DR has been linked to both cardiac autonomic neuropathy and diabetic peripheral neuropathy.
Nephropathy
DR is a strong predictor of the progression of nephropathy, ultimately leading to a decline in kidney function.
Cognitive Impairment
There is emerging evidence suggesting a link between DR and the development of cognitive impairment and dementia.
Macrovascular Complications
Individuals with DR are also more susceptible to macrovascular complications, including cardiovascular disease, stroke, and peripheral artery disease.
A Call for Awareness and Action
DR is a significant public health concern. Raising awareness of the disease, promoting early detection through regular eye exams, and providing comprehensive care are crucial for preventing vision loss and improving the quality of life for individuals living with diabetes. By taking proactive steps and embracing preventive measures, we can effectively combat the growing threat of DR and protect the vision of millions worldwide.