An epilepsy drug has shown promise as a medication for obstructive sleep apnoea, according to trial results presented at the European Respiratory Society Congress this week.
A decades-old epilepsy drug could help curb the symptoms of sleep apnoea, according to new research presented in Vienna this week.
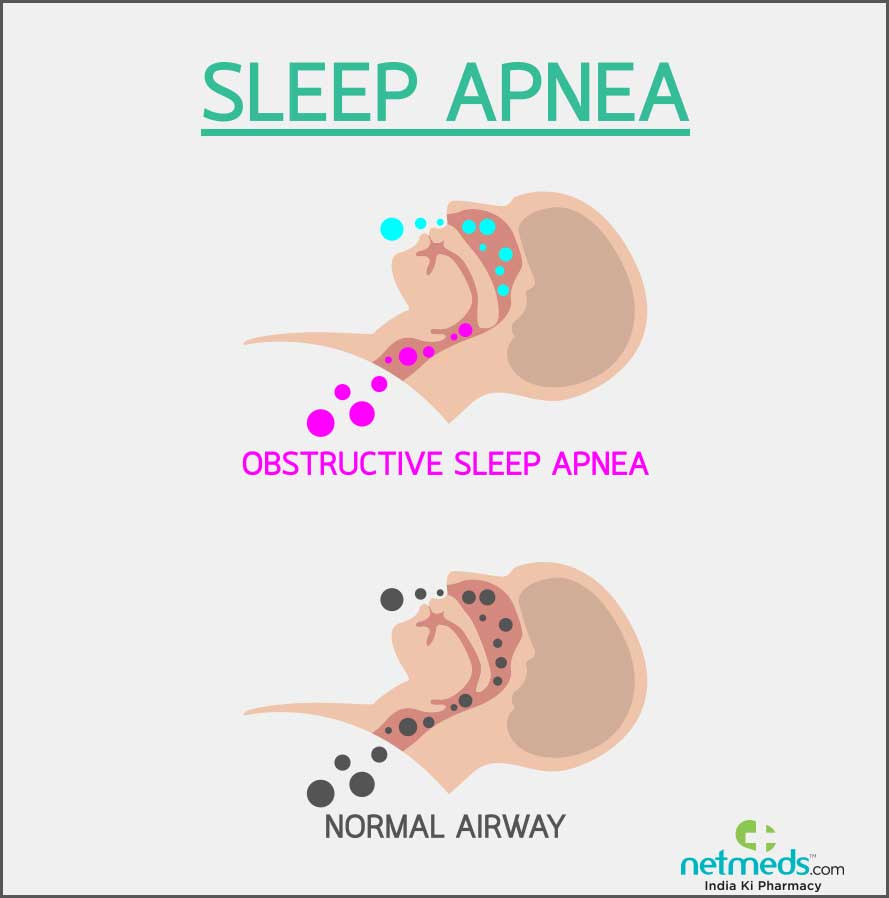
Sleep apnoea – a condition that causes people’s breathing to start and stop many times during sleep, affecting their oxygen levels – affects an estimated 936 million people worldwide, with moderate to severe cases affecting about 425 million people.
Many people with sleep apnoea use continuous positive airway pressure (Cpap) machines to help prevent them from snoring, but they aren’t a silver-bullet solution.
“The standard treatment for obstructive sleep apnoea is sleeping with a machine that blows air through a face mask to keep the airways open,” Jan Hedner, the study’s lead author and a professor of respiratory medicine at Sahlgrenska University Hospital in Sweden, said in a statement.
“Unfortunately, many people find these machines hard to use over the long term, so there is a need to find alternative treatments”.
The study included nearly 300 people in the Czech Republic, Belgium, France, Germany, and Spain who have obstructive sleep apnoea (OSA) – a common form where the throat muscles relax and prevent airflow into the lungs – and did not use Cpap machines.
Researchers gave them either the drug sulthiame, which stimulates muscles in the upper airways, or a placebo.
Over the next 12 weeks, they tracked the participants’ breathing, blood oxygen levels, heart rhythm, eye movements, and brain and muscle activity while asleep.
They found that people taking the drug were less likely to have their breathing stop and had higher blood oxygen levels while asleep compared with those who got the placebo. They were also less likely to be sleepy during the daytime.
Bhik Kotecha, consultant ear, nose and throat surgeon at Nuffield Health Brentwood Hospital, Essex, said lifestyle changes such as weight loss and reduced alcohol intake could also help with sleep apnoea.
Professor Kotecha described sleep apnoea as a condition in which a patient stops breathing momentarily, but repeatedly, during sleep.
He said: “The main symptoms of sleep apnoea include snoring, poor and fragmented sleep, periodic gasping for breath, morning headaches and daytime sleepiness.”
Ms Hedner found after 12 weeks, those taking Sulthiame had up to 50% fewer occasions where their breathing stopped and higher levels of oxygen in their blood during sleep.
After 12 weeks of treatment, participants who took sulthiame were found to have fewer breathing pauses and higher oxygen levels in their blood while sleeping. This suggests that sulthiame may be a viable option for those who find CPAP uncomfortable or ineffective.
A common misconception is that snoring and sleep apnoea are the same thing.
“Snoring occurs as a result of a turbulent airflow and can affect both children and adults,” explained Mr Kotecha.
“If the airway becomes constantly obstructed, then the patient could develop sleep apnoea.”
Children often snore due to enlarged tonsils and adenoids.
“There is a plethora of evidence that demonstrates that the removal of tonsils and adenoids in these children dramatically improves their quality of sleep as well as their cognitive function,” said Mr Kotecha.
“In adults, the problem could be due to an obstruction in the nose as a result of a deviated nasal septum or nasal polyps.
“More commonly, it is the redundant, floppy soft palate in the throat that is the culprit.”
But, because the majority of symptoms happen when asleep, it can be hard to detect.
As the effects of Sulthiame need to be investigated further, Mr Kotecha said there were other ways to treat the condition.
Options included nasal CPAP (continuous positive airway pressure), oral appliances, nasal sprays, antihistamines and lifestyle changes like weight loss and reduced alcohol intake.
Surgeries such as minimally invasive radiofrequency surgery, tonsillectomy and laser or robotic surgery can also be offered to select patients.
“Minimally invasive radiofrequency surgery can improve the upper airway by shortening and stiffening the soft palate, reducing the bulkiness of the tongue and improving nasal patency,” added Mr Kotecha.
A higher dose seemed to make a bigger difference. Patients on the highest dose of sulthiame had 39.9 per cent lower frequency of breathing pauses during sleep, while those on the lowest dose had a 17.8 per cent lower frequency of pauses.
“This suggests that sulthiame could be an effective treatment for OSA, especially for those who find they cannot use the existing mechanical treatments,” Hedner said.
The drug is currently available in European countries as a treatment for childhood epilepsy.
Hedner presented the findings, which have not yet been published in a medical journal, at the European Respiratory Society (ERS) Congress in Vienna, Austria.
While the results are “promising,” more studies are needed to understand the long-term impact of sulthiame and other potential treatments for sleep apnoea symptoms, according to Sophia Schiza, who leads the ERS’s sleep disordered breathing group and is a professor of respiratory and sleep medicine at the University of Crete in Greece.
“Because obstructive sleep apnoea increases the risk of serious health problems such as high blood pressure, heart and metabolic disease, it’s vital that we diagnose and treat the condition,” Schiza, who was not involved in the research, said in a statement.