Imagine being able to take a simple blood test to see if you were at risk for developing a chronic respiratory condition. Thanks to National Institutes of Health (NIH)-funded work being done at UC Davis Health and elsewhere, we are one step closer to this. A new study shows that a blood test may be able to predict how likely a person is to need medical treatment for a lung condition or experience a severe respiratory event. Researchers hope it may lead to earlier intervention and prevention of more serious lung disease.
The paper was published in the American Journal of Respiratory and Critical Care Medicine. It was co-led by a team of researchers from UC Davis Health, Brigham and Women’s Hospital, National Jewish Health, Northwestern University Feinberg School of Medicine, University of Minnesota and Vanderbilt University Medical Center.
“Similar to using cholesterol levels to gauge a patient’s risk for having a heart attack, we’re looking at biological pathways to predict a person’s risk for having a chronic respiratory condition and severe complications from it,” explained study co-author Gabrielle Y. Liu, assistant professor of pulmonology at UC Davis Health. Liu is also a KL2 scholar with the Clinical and Translational Science Center.
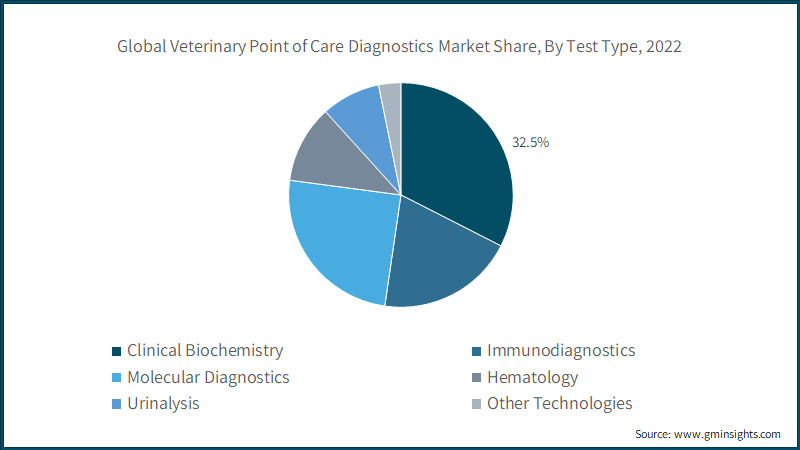
To create the risk score, researchers selected 32 proteins that best predicted which participants were having rapid decline in lung function. These 32 proteins were compiled into a score that was able to predict how likely a person was to either need medical treatment for or die from a lung condition or severe respiratory event.
Adults with higher scores had a 17% increased chance of requiring hospital care for respiratory illness. They also had an 84% increased chance of developing chronic obstructive pulmonary disease (COPD) and at least an 81% increased chance of dying from a respiratory disease, such as COPD or pneumonia. Adults with higher scores also had a 10% increased chance of experiencing respiratory symptoms, such as a cough, mucus, or shortness of breath, which required treatment.
“Our findings that captured patients’ lung function trajectory could potentially be a game changer,” Liu said. “Early detection allows for prompt intervention, potentially preventing the progression of respiratory issues. Timely medical attention can help manage symptoms, improve lung function and enhance overall quality of life.”
To evaluate how well the risk score worked, researchers used it to assess respiratory disease risks in more than 40,000 adults from two earlier observational studies. The prediction model successfully identified adults who had the greatest chance of having severe respiratory conditions after multiple factors, including:
“We are still years away from seeing this type of test used in practice, but it’s a promising advance,” said James P. Kiley, director of the Division of Lung Diseases at the National Heart, Lung, and Blood Institute, a study funder. “It consolidates insights from decades of breathing tests and medical evaluations into a single assessment that has the potential to improve and save lives.”
Liu and her fellow researchers noted this type of blood test still needs to be studied in clinical trials before it could be considered for approval by the U.S. Food and Drug Administration as a screening tool to help predict risks for chronic respiratory diseases.
This study was supported by grants from the National Heart, Lung, and Blood Institute and the COPD Foundation.