A woman claimed to have heard her dead grandmother instructing her to return to her body following a heart attack, according to a study into near-death experiences. Others who were revived after cardiac arrest reported distressing experiences, including the sensation of burning in hell. However, doctors believe that in such cases, the individual's brain may be misinterpreting the medical procedures being performed to save their life.
The researchers involved in this transatlantic study suggested that the man was likely experiencing a burning sensation due to a "tissued" potassium intravenous line, where the fluid was leaking into his muscle instead of entering his bloodstream. These findings have only strengthened a British doctor's belief that something within humans persists even after the body has ceased functioning and died.
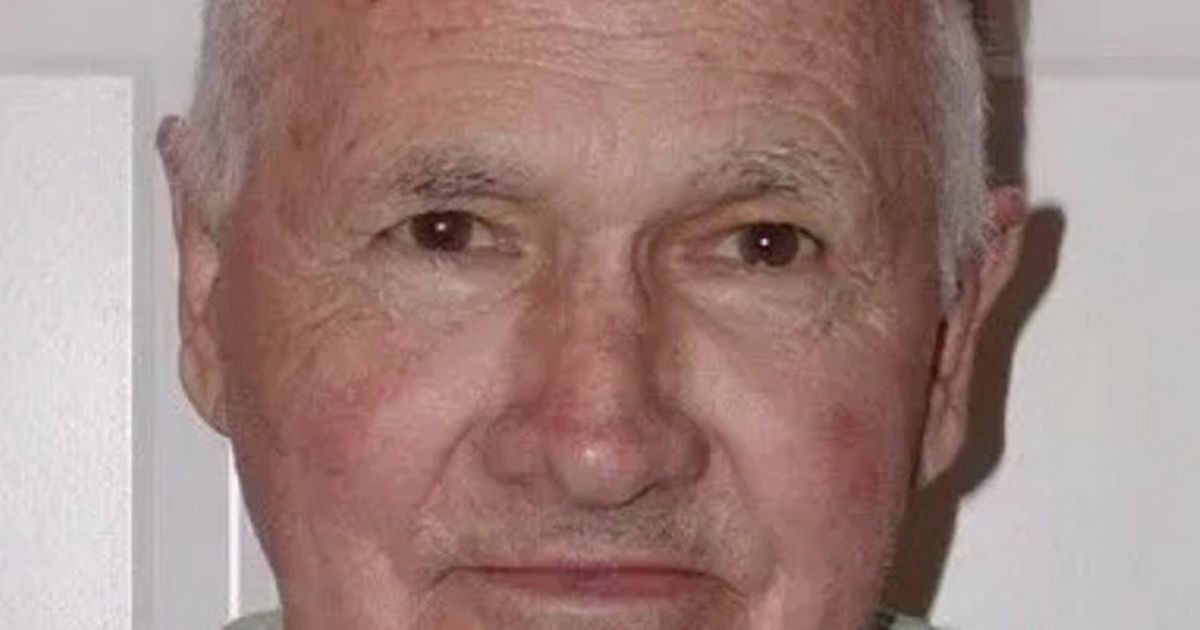
Dr Sam Parnia has been investigating what occurs post-death for 25 years, having developed a quiet fascination with the subject while studying medicine in London. The graduate of Guys and St. Thomas' Medical School presented his findings from the Aware II study at the American Heart Association's Scientific Sessions in Chicago in 2022.
The data was gathered from a combination of interviews with individuals from 25 UK and US hospitals who had survived due to intervention after suffering a heart attack, as well as people self-reporting their experiences following their cardiac arrest. A groundbreaking study has revealed that out of 567 interviewees, just 28 had memories after suffering heart attacks - only these individuals could share their experiences. According to Medical News Today, an alarming 90 per cent of cardiac arrest victims ultimately passed away.
Of those who did retain memories, six reported transcendental moments. Three experienced dream-like visions, including peculiar encounters with a singing fisherman. One person recounted a slowed perception of time, reflecting on their life's impact and love shared with others. Others felt they were journeying towards a place they considered home.
One woman, according to MNT, felt urged by a long-passed grandmother to return to her living body, while a man believed he was enduring the flames of hell. Dr Parnia, an associate professor at NYU Langone Health stationed in the US since 2005, indicated that this research implies human consciousness may not immediately cease post-mortem.
He stated: "These recalled experiences and brain wave changes may be the first signs of the so-called near-death experience, and we have captured them for the first time in a large study. Our results offer evidence that while on the brink of death and in a coma, people undergo a unique inner conscious experience, including awareness without distress."
The intensive care physician said the experiences people recalled "cannot be considered a trick of a disordered or dying brain, but rather a unique human experience that emerges on the brink of death". For him, death gives a rare insight into the depth of the brain's power and ability to store memories.
"As the brain is shutting down, many of its natural braking systems are released," he said. "Known as disinhibition, this provides access to the depths of a person's consciousness, including stored memories, thoughts from early childhood to death, and other aspects of reality.
"While no one knows the evolutionary purpose of this phenomenon, it clearly reveals intriguing questions about human consciousness, even at death," said Dr Parnia, who also studied at Southampton University.
Near-Death Experiences: Common Yet Often Undiscussed
Near-death experiences, also known as NDEs, are extremely common. In fact, as many as 1 in 5 people who almost die in a medical facility report having one — if they are asked. However, only 2% self-report if not asked. This discrepancy highlights a crucial point: many individuals who have NDEs are reluctant to discuss their experiences due to fear of being dismissed or labeled as mentally unstable.
The Importance of Recognizing NDEs in Healthcare
In 2017, Missouri Medicine became the first medical journal to publish a comprehensive physician-oriented study of this well-documented phenomenon. Doctors are generally not trained to recognize or treat these experiences. Consequently, the journal’s articles generated a great deal of international attention — so much so that Missouri University Press subsequently published an expanded version in book form. “The Science of Near-Death Experiences,” which I edited, remains a primary source for educating doctors about NDEs as a frequent and important medical syndrome.
A Real-Life Example: A Patient's Journey Through NDE
A recent case I know about tells a familiar story: A 48-year-old patient was having an exploratory surgery at North Kansas City Hospital. His liver was inadvertently lacerated, and he went into hemorrhagic shock, complicated by uncontrolled bleeding and cardiac arrest. He was at the point of death for 40 minutes and was defibrillated several times, but he survived. He spent 45 days in the hospital, with more than 10 of them in the intensive care unit.
While in the ICU, he told his physicians and nurses, “When I was dead, I went to heaven.” They told him he imagined that trip, which they said was the result of his brain being deprived of oxygen. They told the patient not to tell anyone about his “hallucination,” warning that others would think he had suffered brain damage. This illustrates how medical professionals often dismiss NDEs as mere hallucinations, hindering open communication and potentially causing emotional distress for patients.
Seeking Validation and Understanding
In a subsequent trip to see relatives in Italy, he told physicians there about his experience. They confirmed he had had a near-death experience — and told him they are common, and that most people lose their fear of death and live better lives after having one. This positive response from Italian physicians is a stark contrast to the dismissive attitude he received in the United States. It highlights the need for broader understanding and acceptance of NDEs within the medical community.
A Profound Impact on the Patient
Later, at a neighborhood picnic back in Kansas City, the patient told me about his NDE. He said he had suddenly felt at peace, left his body and looked down to see surgeons and nurses pumping blood into both his arms. He entered a tunnel of light and “went to heaven,” where he was greeted by his mother. There, he also met and became one with the deity, whom he described as a brilliant ball of loving light.
He had been raised Catholic, telling me: “Heaven is everything I hoped it would be and more. I can’t begin to describe how at peace I was.” During this experience, his mother told him it was not his time, and that he had to go back to Earth — but they would be together again not too far in the future.
This patient said, “We have nothing to fear when we die.” He was upset that his American physicians and nurses did not believe him. This experience demonstrates how NDEs can have a profound impact on individuals, often leading to a shift in their perspective on death and life. However, when these experiences are dismissed, it can lead to frustration and a sense of isolation.
The Importance of Validation and Support
If physicians and health personnel tell those who have near-death experiences that these life-changing events are imagined and advise them, “Don’t talk about it or people will think you are not of sound mind,” they create consequences that often adversely affect patients and their families for the rest of their lives. This statement underscores the critical role of validation and support in the aftermath of NDEs. Patients need to feel heard and understood, not dismissed or silenced. Failure to acknowledge and support these experiences can have long-lasting negative consequences.
Providing the Right Care for NDE Patients
Proper medical treatment is simple and forthright: systematic inquiry about having NDEs in people who return from the brink of irreversible death, sympathetic listening and validation, education of the patient and their family about those experiences, and finally appropriate referral to support groups, national NDE organizations and thoughtful study of the many excellent books on the topic. This outlined approach provides a framework for addressing NDEs in a sensitive and compassionate manner, allowing patients to process their experiences and find support from others who understand.
Exploring the Neural Mechanisms of NDEs
Recent research published in NeuroImage suggests that dream-like episodes might be more common during fainting than previously thought. By carefully monitoring brain activity in a group of healthy volunteers during induced fainting episodes, researchers discovered that certain slow-frequency brain waves, particularly in the delta and theta bands, seemed to be linked with the emergence of these extraordinary mental states, which were marked by visions of otherworldly places, a sense of detachment from the body, and intense euphoria.
Insights from Fainting: A New Perspective on NDEs
The findings offer new insights into the neural mechanisms that might underlie near-death experiences, traditionally associated with life-threatening situations like cardiac arrest. Fainting, or syncope, is a common occurrence that can happen to anyone, often triggered by a temporary reduction in blood flow to the brain. While the physical aspect of fainting is well-documented, the subjective experiences that sometimes accompany it have largely been overlooked in scientific literature. Reports of people experiencing vivid dreams, dissociative symptoms, or even out-of-body experiences during fainting have been rare and often dismissed due to their mystical nature.
A Deeper Understanding of Brain Activity During Fainting
The researchers behind this study aimed to fill this gap in knowledge. They wanted to explore whether these fainting episodes could induce experiences similar to near-death experiences and, more importantly, to identify the brain activity associated with these phenomena. By doing so, they hoped to gain a deeper understanding of the neurobiological processes that might contribute to the intense and often life-changing experiences reported by people who have been near death.
The Study's Design and Methods
“It was purely by chance that I began working on this topic. I originally wanted to pursue research in human consciousness, and my thesis advisor proposed this intriguing subject,” said study author Charlotte Martial, a postdoctoral researcher at the Coma Science Group at the University of Liège. “I immediately fell in love with it and have been passionate about it ever since. At the start of my PhD a decade ago, a pivotal encounter with someone who had experienced a near-death experience sparked my deep interest in these fascinating and life-transforming episodes.”
For their study, the research team recruited 22 healthy volunteers, all of whom underwent a thorough medical examination to ensure they had no underlying health conditions that could affect the study’s outcomes. The participants were then asked to induce fainting using a method known as the Valsalva maneuver, a technique that involves trying to exhale forcefully with the nostrils and mouth closed, which temporarily reduces blood flow to the brain.
As the volunteers fainted, their brain activity was closely monitored using a high-density electroencephalogram (EEG), a tool that records electrical activity in the brain using 256 sensors placed across the scalp. This setup allowed the researchers to capture detailed information about the brain’s activity during the moments of induced syncope. After the participants regained consciousness, they were asked to recall and describe any memories or experiences they had during the fainting episode.
Unveiling the Subjective Experiences of Fainting
Over a third of the participants reported experiencing vivid, dream-like episodes during their fainting spell. These experiences included accelerated thoughts, out-of-body sensations, visions of past events, and a sense of entering a different, often extraterrestrial world. Some even reported auditory hallucinations and feelings of euphoria. These experiences closely resembled what are commonly referred to as near-death experiences.
“Our study reveals that it’s not uncommon for people who faint to report rich subjective experiences that may resemble near-death experiences,” Martial told PsyPost. “We demonstrated that dreamlike experiences, characterized by extraordinary and mystical aspects, can emerge during syncope episodes. More broadly, this is one of many states where a person might be considered ‘unconscious’ due to outward unresponsiveness, while in reality, they are experiencing vivid conscious experiences.”
The Neurological Correlation: Slow-Frequency Brain Waves
On the neurological side, the EEG data revealed specific patterns of brain activity that appeared to be linked with these experiences. During the fainting episodes, the researchers observed surges in slow-frequency brain waves, particularly in the delta and theta bands. These types of brain waves are usually associated with deep sleep or meditation and are rarely prominent in a fully awake state. The presence of these waves suggested that the brain was in a state of disconnected consciousness—where the person is unresponsive to the external environment but may still be experiencing vivid internal sensations.
“I was quite amazed to discover the strong positive correlations we observed between cortical activity associated with theta and delta waves and the richness of subjective experience in specific regions of interest, such as the insula, temporoparietal junction, cingulate cortex, and parahippocampal gyrus — areas known to be crucial for self-awareness and the (sometimes distorted) perception of our body.”
Unraveling the Mystery: Delta Waves as a Potential Marker
Interestingly, the intensity of these experiences seemed to be predicted by the amount of delta activity observed during the fainting episode. This finding led the researchers to propose that delta waves could be a marker of the brain’s potential to generate such extraordinary conscious states, even when disconnected from the outside world.
A Breakthrough in Research: New Avenues for Understanding NDEs
“Our study is the first to explore the electrical brain activity of individuals using high-density EEG during syncope,” Martial explained. “We found that these dreamlike experiences, some of which may carry the hallmarks of near-death experiences, appear to be supported by surges in slow-frequency activity bands on EEG. While these findings should be interpreted with caution, they open up new avenues for understanding the neurobiological mechanisms underlying near-death-like experiences.”
Looking Ahead: Improving Patient Care and Consciousness Detection
The long-term goal of this research is to understand the brain mechanisms behind near-death experiences, with the aim of improving patient care and developing tools to detect consciousness in unresponsive individuals.
“From a scientific perspective, this line of research aims to demonstrate, across a comprehensive spectrum of physiological, pathological, and pharmacological conditions, that unresponsiveness cannot be considered a surrogate for unconsciousness,” Martial said.
A Holistic Approach to NDEs: From Research to Clinical Application
“From a clinical perspective, my long-term goal is to search for markers of near-death and near-death-like experiences in different clinical conditions to develop a comprehensive neurophysiological model for these experiences. My ultimate objective is the improvement of patient outcomes. Indeed, we now understand that encountering such mystical and extraordinary experiences in unexpected situations can have significant implications.”
Potential for Therapeutic Applications: A New Era of Understanding
“I’m optimistic that our research could inform therapeutic follow-up for near-death experience patients and lay the groundwork for innovative strategies that use these markers for the automated detection of conscious experiences, without relying solely on memory, ultimately assisting medical management.”
The Study's Authors and Key Findings
The study, “EEG signature of near-death-like experiences during syncope-induced periods of unresponsiveness,” was authored by Charlotte Martial, Andrea Piarulli, Olivia Gosseries, Héléna Cassol, Didier Ledoux, Vanessa Charland-Verville, and Steven Laureys. The study's findings represent a significant step forward in our understanding of the neurological basis of NDEs and hold great promise for improving patient care and advancing our knowledge of human consciousness.
The Importance of Ethical Considerations in Research
I found the news story “Psychedelic drugs may give a glimpse into near-death experiences” in the Aug. 27 Star interesting, especially in its unique and insightful study of individuals who have both had a NDE and used psychedelic drugs. Conversely, disturbing was the story’s mention of the intentional use of psychedelic drugs as “a powerful tool to study near-death experiences” in otherwise healthy people, as proposed by Dinesh Pal, an associate professor at the University of Michigan.
A Risky and Unethical Approach: Inducing NDEs in Healthy Individuals
I find this practice dangerous and unethical. As many as 10% of NDEs are “distressing” and like a visit to hell, patients report. They terrify some people for life. It would be tragic and indefensible to induce even one of these upsetting experiences in a healthy human being used as a guinea pig. This argument emphasizes the crucial need for ethical considerations in research, especially when dealing with potentially traumatic experiences like NDEs. It is imperative to prioritize the well-being of research participants and avoid subjecting them to unnecessary risks or distress.
The Potential Risks of Psychedelic Drugs
Like any medication, psychedelic drugs can have adverse reactions, some serious. While they offer great promise for treatment of a variety of mental disorders, if properly used and studied, their side effects and long-term consequences have not been fully delineated. These risks may be appropriate for people with major psychiatric disorders, but not for researchers with idle curiosity about near-death experiences to experiment on healthy, normal people. This statement highlights the complex nature of psychedelic research, acknowledging its potential benefits while emphasizing the need for caution and responsible use, especially when considering the potential risks involved. The ethical implications of using these substances in research are paramount and must be carefully weighed against the potential benefits.
The Importance of Ethical Research Practices
Such research is risky and serves no ethical purpose. Doctors, first do no harm. This concluding statement reiterates the fundamental principle of medical ethics, reminding us that the well-being of patients must always be prioritized. It underscores the importance of ethical research practices that ensure the safety and well-being of participants and avoid unnecessary risks.
A Call for Responsible Research and Compassionate Care
John C. Hagan III is editor of Missouri Medicine: The Journal of the Missouri State Medical Association and the book “The Science of Near-Death Experiences.” He is former president of the Kansas City Medical Society, the Missouri Society of Eye Physicians & Surgeons and the Clay-Platte County Medical Association. This biography provides context for the author's expertise and involvement in the field of NDE research. It emphasizes his commitment to promoting understanding and ethical practices within the medical community.